Questions to Discuss with Your Surgeon
- What is the goal of the recommended treatment (curative or palliative)?
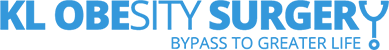
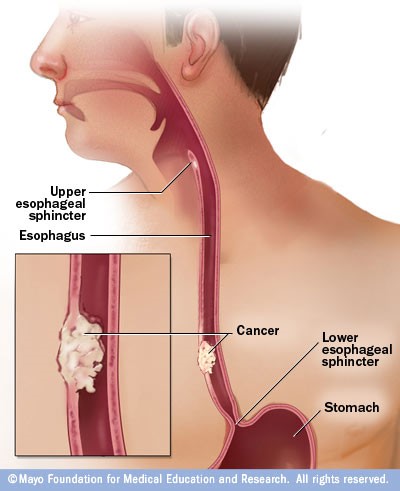
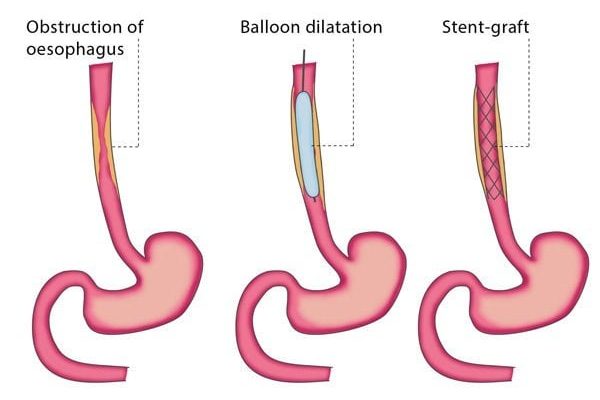
The goal of the recommended treatment depends on the stage and spread of your esophageal cancer. If the cancer is localized and detected early, the goal is often curative, aiming to remove the cancer completely and achieve long-term remission. For advanced-stage cancer that has spread beyond the esophagus, the goal may be palliative, focusing on relieving symptoms, improving quality of life, and prolonging survival.
- What are the chances of success for each treatment option?
The chances of success vary based on the stage of cancer, the specific type of treatment, and individual patient factors such as overall health. For early-stage esophageal cancer, surgery combined with neoadjuvant chemoradiotherapy can significantly increase the chances of cure. For more advanced stages, the success of treatments like chemotherapy and radiotherapy may be measured by the ability to shrink tumors, relieve symptoms, and extend survival. Your surgeon can provide statistics based on your specific situation.
- What are the potential risks and side effects?
Each treatment comes with its own set of risks and side effects:
– Surgery: Risks include bleeding, infection, reactions to anesthesia, and complications such as leakage at the surgical site, respiratory issues, and changes in swallowing.
– Chemotherapy: Common side effects are nausea, vomiting, fatigue, increased risk of infection, hair loss, and organ-specific toxicities.
– Radiotherapy: Side effects may include skin irritation, fatigue, difficulty swallowing, and potential long-term damage to surrounding tissues and organs.
Your surgeon will discuss the specific risks associated with the recommended treatments for your case.
- How long will the treatment and recovery take?
The duration of treatment and recovery depends on the treatment plan:
- Chemoradiotherapy: Typically lasts several weeks, often around 5-6 weeks for radiation, combined with chemotherapy cycles.
- Surgery: Hospital stay can range from 7 to 14 days, with full recovery taking several months. Minimally invasive procedures may reduce recovery time. However, any surgical complication will cause prolonged hospital stays due to further surgery/ intervention to address the complications.
- Combined Treatments: If you undergo neoadjuvant chemoradiotherapy followed by surgery, the overall process from start to full recovery could span several months to a year.
Your surgeon will provide a more precise timeline based on your treatment plan.
- How will each treatment affect my daily life?
The impact on daily life varies:
- Chemotherapy: You may experience fatigue, nausea, and other side effects that can limit daily activities. Maintaining nutrition and managing side effects will be important.
- Radiotherapy: Fatigue and swallowing difficulties might impact eating and daily routines.
- Surgery: Post-surgery, you will need time to recover, adapt to changes in eating habits, and gradually return to normal activities.
- Support from healthcare professionals, family, and friends will be essential during treatment and recovery.
- What kind of follow-up care will be needed?
Follow-up care typically involves regular check-ups to monitor for recurrence, manage any ongoing side effects, and ensure overall health. This may include:
- Physical exams
- Imaging tests (CT scans, PET scans)
- Endoscopies
- Blood tests
- Nutritional support and dietary adjustments
- Rehabilitation and physical therapy
Your surgeon will outline a specific follow-up schedule tailored to your needs.
- Are there any clinical trials available?
Clinical trials may offer access to new treatments that are not yet widely available. These trials can be an option if standard treatments are not suitable or if you are interested in contributing to medical research. Your eligibility for clinical trials will depend on factors such as the stage of your cancer, previous treatments, and overall health. Your surgeon can provide information about any relevant clinical trials and help determine if you are a good candidate.