What is Diabesity (Obesity + Diabetes)
Obesity, insulin resistance, metabolic syndrome and type 2 diabetes have reached epidemic proportions worlwide. You might be affected by these conditions, either directly or indirectly.
Diabesity (diabetes + obesity) is used to describe them. Diabesity can be defined as a metabolic dysfunction that ranges from mild blood sugar imbalance to full-fledged type 2 diabetes with a constellation of signs that includes:
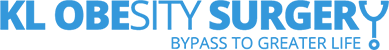
- Abdominal obesity (i.e. “spare tire” syndrome);
- Dyslipidemia (low HDL, high LDL and high triglycerides);
- High blood pressure;
- High blood sugar (fasting above 100 mg/dL, Hb1Ac above 5.5);
- Systemic inflammation
It affects more than one billion people worldwide. Malaysia has the highest number of diabetics in Asean with an estimated more than 3.6 million adults affected. Diabesity may already be the leading cause of chronic disease and death in the world, and its impact is expected to rise dramatically in the next 25 years.
Approximately 90 percent of all diabetics in the word are type 2 diabetics (T2DM). T2DM is the form of the disease most closely linked to obesity and thus the name, Diabesity has been used to describe this association.
In this form of diabetes, the body does not produce enough of the hormone insulin, or the cells in the body do not use insulin properly. Insulin is necessary for the body to be able to use glucose or blood sugar for energy. As a result, glucose builds up in the blood, where it can wreak havoc, instead of going into cells. Complications of diabetes include heart disease, blindness, nerve damage and kidney damage.

How is Type 2 Diabetes normally treated?
Traditionally, lifestyle changes including losing excess weight, eating a healthful diet and engaging in regular exercise are the first-line treatments for type 2 diabetes. When these modifications do not make enough of effect in the disease, medications can be prescribed. Some medications help the pancreas produce more insulin, while others help the body use the insulin that it does produce more efficiently. If these drugs don’t work, a person may need to take insulin. However, study has shown that most people need multiple anti-diabetic drugs to fight this deadly disease in the long run.
Does Metabolic Surgery “Cure” Diabetes?
More than 30 scientific studies say yes!
To be crystal clear, diabetes is poorly understood and medical science cannot claim a “Cure”. The aim is to put it in remission, defined as normal blood sugar levels and no need for diabetes medication. This means bringing glucose to normal levels and arresting the progression of the diabetic complications, thus giving the body a chance to repair the damage.
- A landmark 2004 study in JAMA of more than 22,000 people who underwent bariatric surgery showed the following:
- Diabetes was completely resolved or improved in 86% of patients.
- High blood lipids improved in 70% or more of patients.
- High blood pressure was resolved or improved in 78% of patients.
- A study in the Annals of Surgery showed that 83 percent of 240 people who underwent gastric bypass were “cured” of their diabetes.
- A study in the New England Journal of Medicine found that long-term mortality after gastric bypass surgery was significantly reduced, particularly deaths from diabetes.
The bottom line is that metabolic surgery can play a big role in treating Type 2 diabetes.
How Does Metabolic Surgery “Cure” Type 2 Diabetes?
We know that metabolic surgery puts type 2 diabetes into remission; what we don’t know is how it does it.
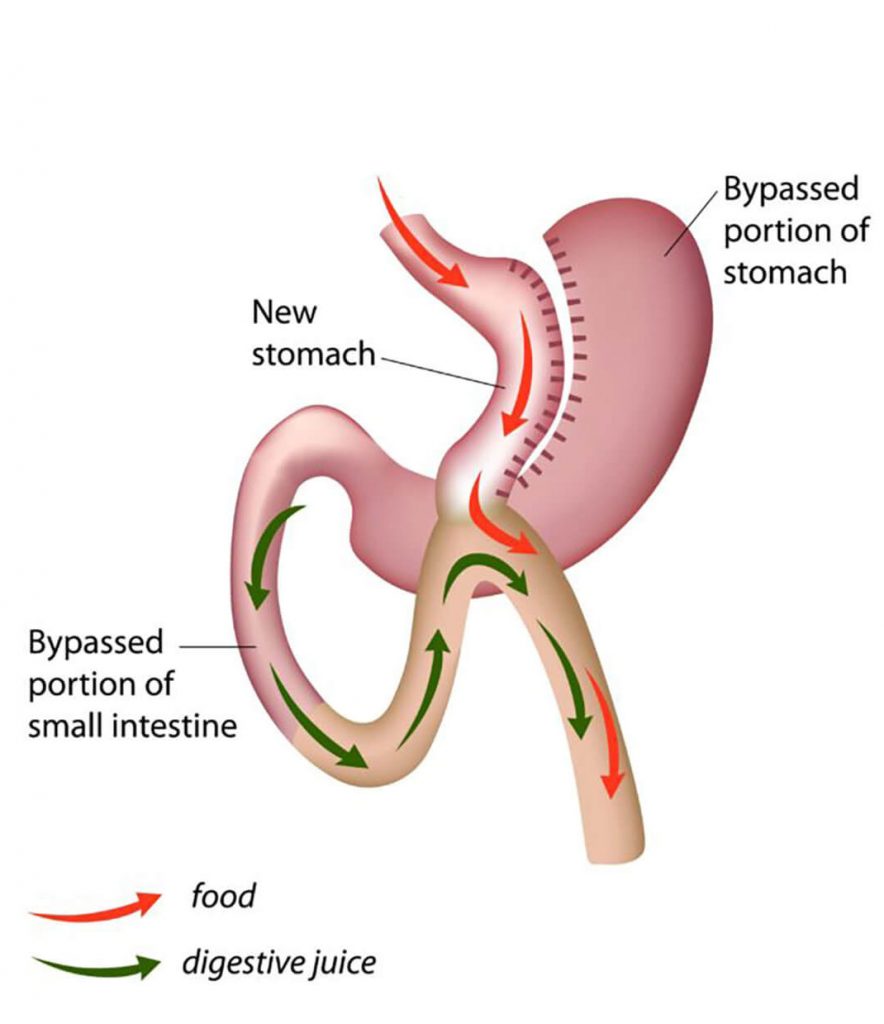
Some theories do exist, including the idea that shunting food directly to the lower intestine stimulates a substance called glucagon-like peptide 1 (GLP-1) , which can increase insulin production.
Another theory suggests that hormones that prompt hunger such as peptide Y (PPY) may be dulled by rearranging the anatomy of the gut, so if they crave less sugar, people may be able to manage their blood sugar levels better.
We also do not know the ideal type of metabolic surgery for treating diabetes. Studies have looked at different types of surgeries. Until the right one is found, the laparoscopic RY gastric bypass is the one that works well and puts type 2 diabetes into remission almost immediately after the surgery.
Another question that remains is when should the surgery be performed — when diabetes is first diagnosed or down the road, when complications have already begun to arise? Intuitively, the sooner the better to prevent the complications of type 2 diabetes.
Aim I eligible for Metabolic surgery
Actually, 2/3 of the world’s type 2 diabetics are not morbidly obese. They are however, overweight with BMI range 27-35. Most metabolic surgeons with a lot of experience, will accept patients with type 2 diabetes and BMI of 30 or greater for metabolic surgery
Generally, you are eligible for metabolic surgery if you have:
- Central obesity with waist circumference > 90cm
- BMI> 30
- Poorly controlled diabetes despite on optimal medication (HbA1C > 7)
- Fatty liver/ non-alcoholic liver disease
What type of Metabolic surgery?
Generally, different type of metabolic surgery has its merit, risk and chance of diabetic remission after surgery, the surgeon will evaluate you and choose the most suitable metabolic surgery to ensure best outcome.
Sleeve gastrectomy
Roux-en-Y gastric bypass

Mini- gastric bypass
You can discuss all of these metabolic surgeries and which one is best for you at the clinic consult with Metabolic surgeon, Dr. Pok Eng Hong