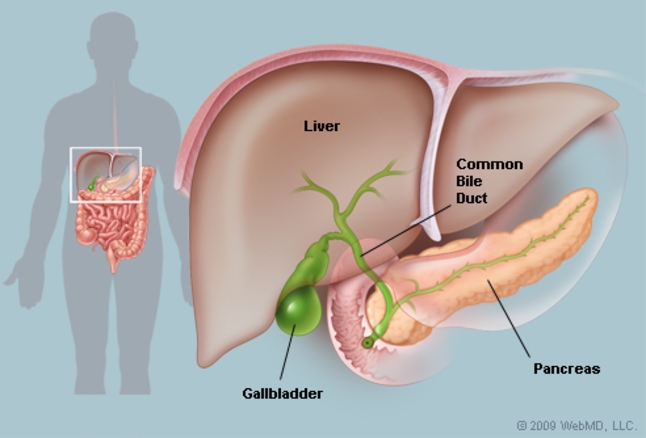
Function of gallbladder and bile juice
- Bile is a fluid made in the liver and contains various substances including bile pigments, bile salts, cholesterol and lecithin.
- passed into tiny tubes called bile ducts. The bile ducts join together (like the branches of a tree) to form the main bile duct.
- constantly drips down the bile ducts, into the main bile duct, and then into the gut after the stomach.
- The gallbladder lies under the liver on the right upper side of the abdomen, like a pouch which comes off the main bile duct and fills with bile. It is a ‘reservoir’ which stores bile.
- The gallbladder contracts (squeezes) when we eat, thus empties the stored bile back into the main bile duct, passes along the remainder of the bile duct into the duodenum (the first part of the gut after the stomach).
- Bile helps to digest food, particularly fatty foods.
ACUTE CHOLECYSTITIS
The medical term for gallstone formation is cholelithiasis.
- Cholecystitis is an inflammation of the gallbladder, which can happen suddenly (acute) or over a period (chronic).
- Most cases are caused by gallstones.
- When a gallstone becomes stuck in the cystic duct (this is the tube that drains bile out from the gallbladder into the bile duct), bile then builds up in the gallbladder, which becomes stretched (distended).
- The walls of the gallbladder become inflamed, and in some cases the inflamed gallbladder becomes infected.
- An infected gallbladder is more prone to lead to complications.
- The inflammation may settle down with treatment.
- However, removal of the gallbladder is usually advised to prevent perforated gallbladder., which is a condition when the gallbladder bursts or leaks. It happens in rare cases but it is life threatening.
THE COMMON SYMPTOMS OF CHOLECYSTITIS
Sharp pain in the centre or right upper abdomen .
- Low grade fever.
- The pain may radiate (travel) to the back or to the right shoulder and tends to be worse if you breathe in deeply.
- Jaundice (yellowing colour of the skin), may occur if gallstones are in the common bile duct.
- You may also develop nausea (feeling sick) and vomiting
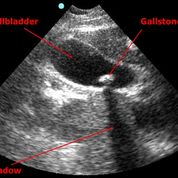
HOW IS CHOLECYSTITIS DIAGNOSED?
- An ultrasound scan is commonly done to clarify the diagnosis
- It can usually detect gallstones, the thickness of gallbladder and surrounding fluid accumulation if the gallbladder is infected
- it can assess the degree of dilatation of bile duct and biliary due to the presence of migrated gallstone causing bile duct obstruction.
WHAT IS THE TREATMENT FOR CHOLECYSTITIS?
- Usually, you will need to be admited for medical therapy ( Iv antibiotic, iv fluids, pain killer, fasting to rest the gallbladder),
- With this initial treatment the gallstone that caused the blockage often falls back into the gallbladder, and the inflammation and symptoms often settle down.
- The gallbladder will usually be removed by surgery for faster recovery, ideally withon 72 hours of oset of symptoms for the ease of surgery.
- Inform your surgeon if you are taking blood thinners ( Aspirin, Plavix, etc) as it can cause bleeding during surgery
- Sometimes the operation is delayed for several weeks until the inflammation has settled.
- Open or laparoscopic techniques to remove the gallbladder may be used depending on various factors.
- Laproscopic surgery is now the most common way to remove a gallbladde and is called laparoscopic cholecystomy.
- Only small cuts are needed in the abdomen with small scars remaining afterwards. The operation is done with the aid of a special telescope and miniature instruments which allow the surgeon to performed surgery inside abdomen through the small cut.
- Some people need a traditional operation to remove the gallbladder, that is called open cholecystectomy which requires abdominal wall incision in difficult gallbladder due to severe scarring or distorted anatomy after long standing inflammation.
LAPAROSCOPIC CHOLECYSTECTOMY SURGERY
Laparoscopic cholecystectomy is considered a minimally invasive procedure because it uses small incisions instead of a large incision in the abdomen. This allows for quicker recovery time and less postoperative pain than open surgery.
During the surgery, the laparoscope is used to view the inside of the abdomen and the gallbladder. Other instruments, such as forceps, scissors, and a cautery device, are inserted through the other incisions to remove the gallbladder.
The procedure can be performed under general anesthesia, which means the patient is asleep during the surgery. After the procedure the patient will have to rest for a period of time, as well as follow a specific diet recommended by the surgeon for a time period.
Patients can expect to have some discomfort, soreness and swelling around the incision site and also may experience some nausea and fatigue, but these symptoms usually improve within a few days after surgery.
The recovery time for laparoscopic cholecystectomy varies from person to person, but most people are able to return to their normal activities within 2-3 weeks after surgery.
It is important to follow the instructions provided by the surgeon to ensure a successful recovery.
Laparoscopic cholecystectomy videon
WHAT ARE THE POSSIBLE COMPLICATIONS /SIDE EFFECTS OF SURGERY?
As with any surgery, there are potential complications associated with laparoscopic cholecystectomy. However, this procedure is considered to be a safe and effective treatment for gallstones.
The most common complications include:
- Infection: Infection can occur at the incision site or within the abdomen. This is typically treated with antibiotics.
- Bleeding: There is a small risk of bleeding during or after the surgery.
- Injury to nearby organs: It is possible that the instruments used during the surgery could accidentally cause injury to nearby organs, such as the liver or the common bile duct.
- Postoperative bile leak: There is a small risk that the ducts that transport bile from the liver to the small intestine can be damaged during surgery resulting in a bile leak that can cause infection, fever and jaundice, requiring additional surgical repair.
- Adhesions: After the surgery, the healing process can cause the tissues in the abdomen to stick together, this is called adhesion, can be managed with medication or another surgery.
- Nausea and vomiting: it is due to effect of general anesthesia which will settle down with medication
- Shoulder pain and: CO2 insufllation during laparoscpic surgery is used to increase the abdominal space available for the surgeon to work and see. it can cause referred pain to the shoulder which last for few days
- Rarely, the gallbladder stones have migrated to common bile duct casusing retained stones in it that need ERCP to remove it after surgery.
- Conversion to open surgery: In some cases, the surgeon may need to switch to open surgery during the procedure if they are not able to complete it laparoscopically due to severe adhesion/technical difficulty. Its is not considered as failure of surgery as it is performed for the safety of patient
Most of these complications are rare and can be treated effectively. The best way to minimize the risk of complications is to choose a surgeon who is experienced in performing laparoscopic cholecystectomy.
It’s important to discuss the potential risks and benefits with your surgeon before the surgery and ask any question you may have.
RECOVERY AFTER A GALLBLADDER IS REMOVED
- You do not need a gallbladder to digest food.
- Bile still flows from the liver to the gut once the gallbladder is removed.
- However, there is no longer any storage area for bile between meals.
- You can usually eat a normal diet without any problems after your gallbladder is removed. your digestion system is still the same
- However, some people who have had their gallbladder removed have some mild abdominal discomfort or bloating from time to time. This may be more noticeable after eating a fatty meal.
WHAT IS THE COST OF GALLBLADDER SURGERY?
The cost of a laparoscopic cholecystectomy can vary depending on a number of factors, such as the location of the surgery, the hospital or clinic where the procedure is performed.
In the Malaysian, the cost can be 20-25k, mind that this cost estimates can vary a lot depending on the location, facility and the insurance plan.
It’s a good idea to check with your insurance company to find out exactly what costs will be covered under your policy, and how much you will be responsible for paying out of pocket. And also to check the cost with the hospital or clinic where the surgery will be performed, as well as any associated costs such as lab tests, prescription drugs, and follow-up care.