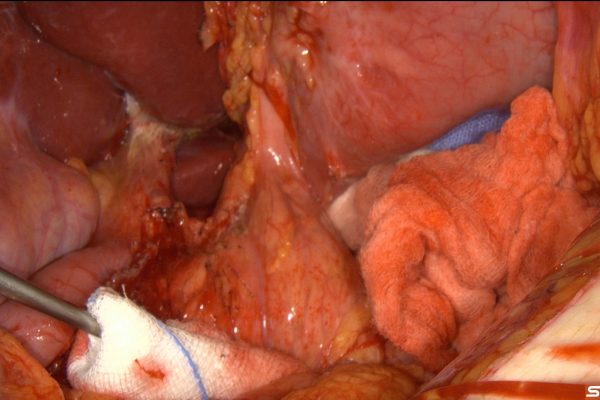
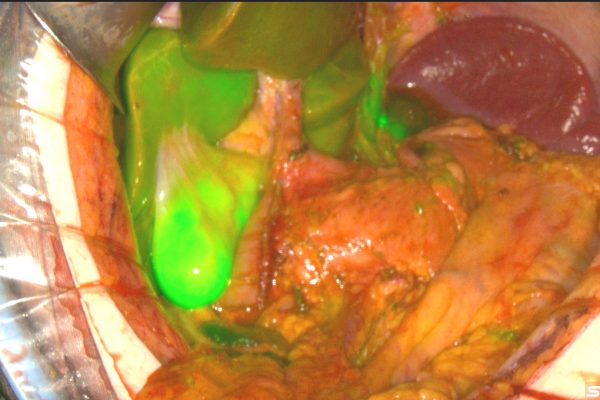
Indocyanine green (ICG) navigation is a technique used in gastric cancer surgery to enhance visualization, enabling surgeons to better identify and preserve vital structures and improve the accuracy of tumor removal. Here’s how it is generally used:
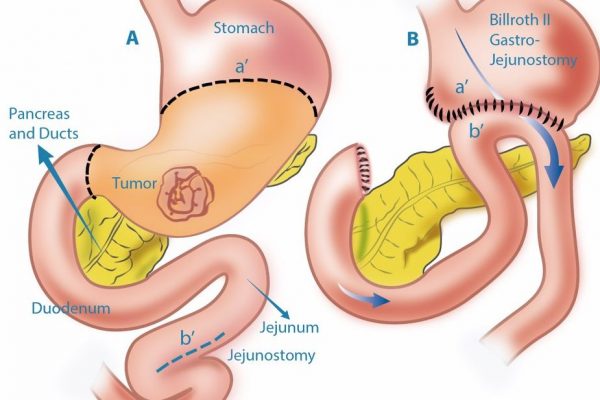
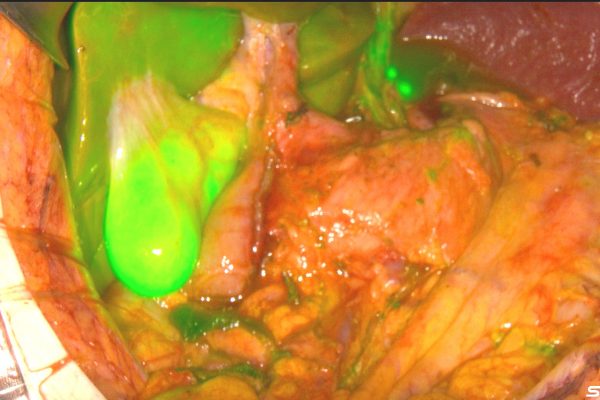
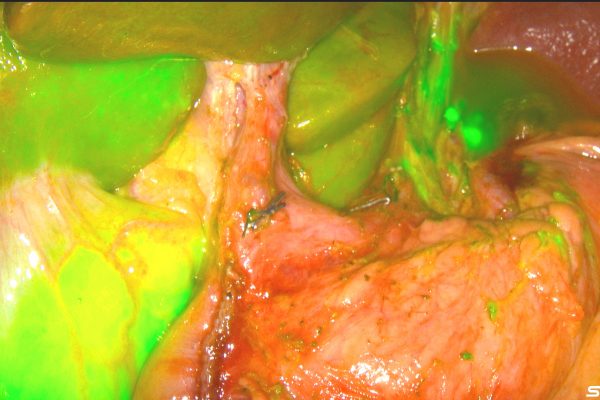
1. Visualization of Blood Flow: ICG, when injected intravenously, binds to plasma proteins and remains within the vasculature. Under near-infrared light, ICG fluoresces, allowing surgeons to assess the blood flow to various parts of the stomach and surrounding tissues. This is crucial to ensure adequate blood supply to tissues, particularly when reconstructing the digestive tract after tumor removal.
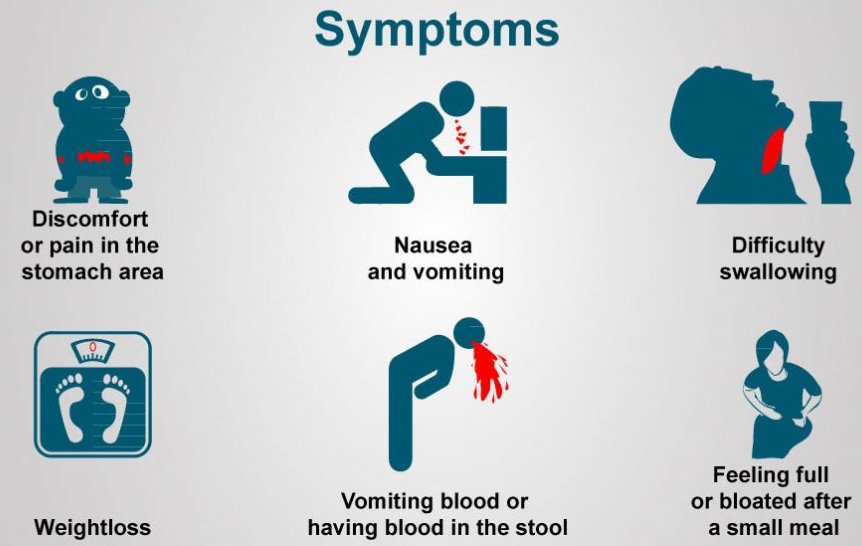
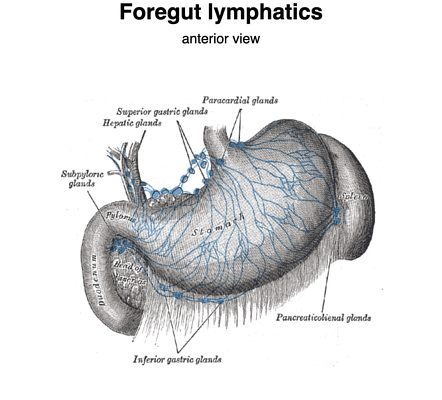
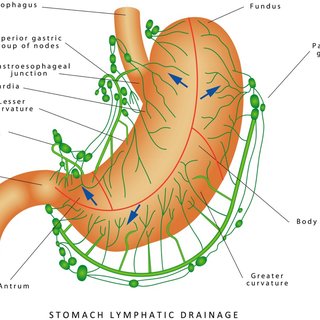
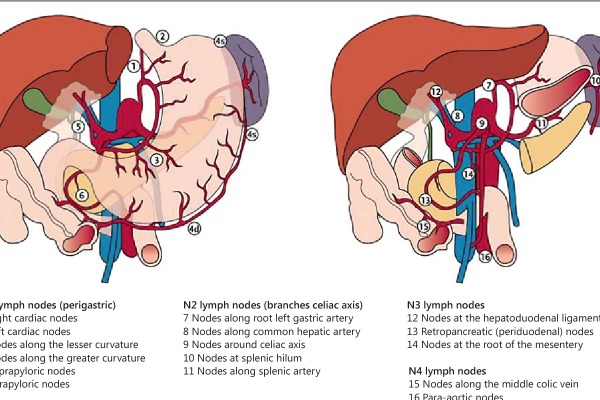
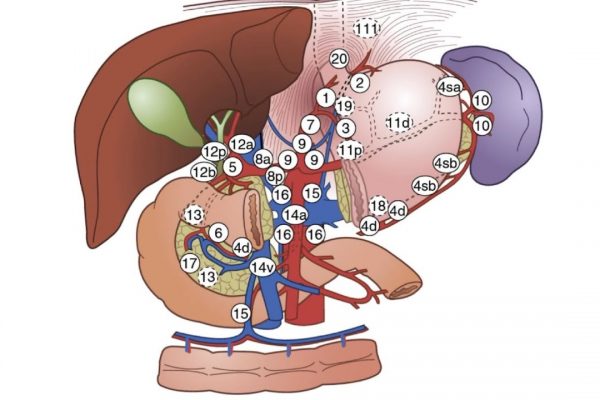
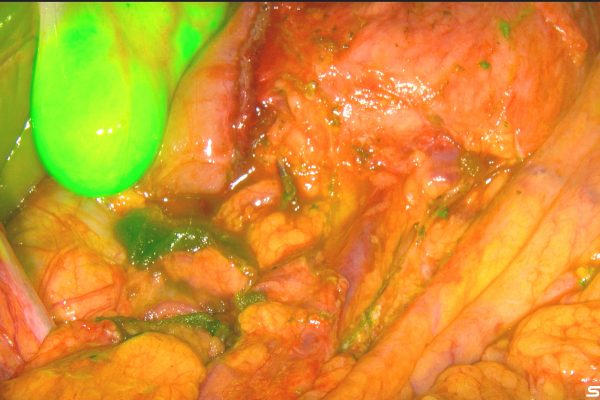
2. Lymphatic Mapping and Sentinel Lymph Node Identification: ICG can help in the mapping of lymphatic drainage from the gastric tumor. This aids in the identification of sentinel lymph nodes (the first lymph nodes to which cancer is likely to spread from a primary tumor). By accurately identifying and analyzing these nodes, surgeons can better assess the spread of cancer and make more informed decisions about the extent of lymph node removal.
3. Tumor Delineation: ICG can assist in delineating the margins of the tumor, helping surgeons achieve a more precise resection with adequate margins, which is critical in reducing the risk of cancer recurrence.
4. Enhanced Visualization in Minimally Invasive Surgery: In laparoscopic and robotic surgeries, ICG navigation provides real-time, enhanced visual feedback that can improve the surgeon’s ability to operate more precisely in a minimally invasive manner.
The use of ICG navigation in gastric cancer surgery has shown potential in improving surgical outcomes by reducing complications, increasing the likelihood of complete tumor resection, and preserving healthy tissue. This technology represents a significant advancement in the surgical management of gastric cancer, contributing to more personalized and effective treatments.